The disease of hyperparathyroidism is diverse. The causes of it are very different. As a simplification there’s primary, secondary and tertiary hyperparathyroidism:
All three of these involves increased PTH (parathyroid hormone)
Primary: elevated calcium, low phosphorus in blood stream. Usually caused by a parathyroid adenoma.
Secondary: normal or low calcium, usually caused by renal failure.
Tertiary: failure of treatment of secondary hyperparathyroidism to correct increased PTH.
More details on hyperparathyroidism
Primary hyperparathyroidism is most commonly caused by adenomas, greater than 85%. Next most common cause would be hyperplasia which is 10% of the causes, and there is a 1% possibility that primary hyperparathyroidism is caused by a carcinoma.
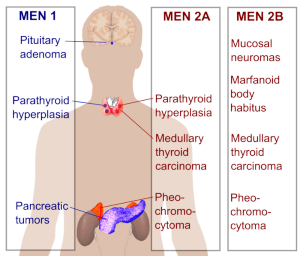
Risk factor for primary hyperparathyroidism includes family history, MEN I and MEN IIa, and also radiation. Major difference between MEN IIA and IIB: MEN IIA has Hyperparathyroidism – hyperplasia, MEN IIB does not. More on MEN syndromes.
Sestamibi scan is a method of detecting hyperparathyroidism.
Carcinomas which are commonly associated with hypercalcemia:
- Breast Cancer Metastasis
- Postate Cancer
- Kidney Cancer
- Lung Cancer
Another cause of hypercalcemia: FHH – Familial hypocalciuric hypercalcemia
- autosomal dominant
- asymptomatic hypercalcemia and low urine calcium
- with or without elevated PTH
- No treatment is generally required for FHH